Initial Steps
Virtual or hybrid provision of medication abortion (MA), which is also called no-touch or low-touch medication abortion, is one where some or all of the appointments are carried out virtually over phone and / or video by reducing or eliminating blood work and ultrasound. The purpose is to reduce patients’ risk of contracting transmissible infections (as in the case of COVID-19) or reduce the need for patients to travel long distances or wait for days or weeks to receive abortion.
As explained elsewhere, virtual and hybrid provision of MA is based on low resource availability and requires a balance between prescribers’ experience, patients’ safety and patients’ needs.
When receiving requests for virtual or hybrid medication abortion, prescribers should[7]:
- Confirm patient identity and ensure patient has privacy and safety to discuss.
- Provide written information on medication and procedural abortion in advance of the consultation.
- If not already done, ask the patient to obtain and take a qualitative urine high sensitivity pregnancy test from the pharmacy.
- Schedule a first virtual visit via telephone or video.
Virtual Assessment
The following assessments should be carried out[7,19]:
- Review pregnancy options counselling.
- Establish pregnancy and gestational age.
- Review date of last menstrual period (LMP) and date of positive qualitative pregnancy test.
- Review relevant medical history, including recent hormonal contraception and risk factors and signs of ectopic pregnancy.
- Exclude contraindications.
- Assess the need for an ultrasound to determine gestational age and the location of pregnancy[5]:
- According to SOGC's protocol on medication abortion via telemedicine, ultrasound should be obtained if LMP is uncertain, LMP is over 70 days, and the signs, symptoms and risk factors of ectopic pregnancy (EP) are present.
- Medication abortion performed without ultrasound is, by definition, pregnancy of unknown location and should be managed accordingly. Though the risk of unrecognized EP is low, close follow-up is required to ensure completion of the medication abortion.
- Assess the need for blood work to measure hemoglobin[7]:
- According to Health Canada, hemoglobin should be over 9.5 g / dL before starting MA.
- Screen patients for increased risk of anemia through a detailed medical history.
- If patients are suspected to have an increased risk of anemia, complete blood count is indicated. Otherwise, measuring hemoglobin is unnecessary.
- Assess the need for blood work to determine Rhesus status (Rh)[7]:
- As explained elsewhere, guidelines on Rh status have been updated and vary between organizations.
- According to the SOGC’s Guideline on Prevention of RhD Alloimmunization published in 2024, for non-sensitized Rh D-negative individuals who have experienced threatened, spontaneous or induced abortion after 12 weeks gestation, administration of 300 μg of Rho(D) immune globulin is suggested.
- The National Abortion Federation, the Society of Family Planning and the World Health Organization all recommend Rh testing and administration for patients who are 12 weeks gestation or beyond, but not for patients who are under 12 weeks LMP.
- Assess the need for STI testing[7]:
- Offer testing for chlamydia and gonorrhea if patients come to office.
- Otherwise, evaluate the risk of STIs and consider remote testing if risk factors are present, and discuss the potential need for antibiotic treatment.
Informed Consent
After the patient and the health provider determine that medication abortion (MA) is the right option, the health provider should[2,6,7,10]:
- Obtain written or verbal informed consent (see examples by CAPS-CPCA platform and the Bay Center for Birth Control) and document it in the patients' chart.
- Prescribe:
- Mifepristone 200 mg (MIFE) orally and misoprostol 800 mcg (MISO) buccally or vaginally (this combination is packaged and branded as Mifegymiso).
- Additional dose of MISO buccally or vaginally in case of incomplete or failed abortion.
- Analgesics and antiemetics as per health provider / facility protocol.
- Antibiotic prophylaxis, if needed, as per health provider / facility protocol.
- Provide instructions on how to take the medication.
- Ensure patients know how to manage side effects and when and where to seek care for complications.
- Consider informing patients if the MA procedure involves off-label, evidence-based practices.
- Much of the MA off-label practices are based on low-resource availability and require a balance between health providers’ experience, patients' safety and patients’ needs.
- It is recommended to inform patients about off-label practices so patients understand the risks involved and understand that off-label practices might vary depending on prescribers’ experience and comfort level.
- Discuss post-abortion contraception options. Emphasize that patients can quickly return to fertility following the abortion.
- Set up follow-up appointment(s), either in-person or via phone/video. Do discuss any safety or privacy plan if needed.
- Provide patients with patient instruction manuals (see an example by the SHORE center and the Planned Parenthood Ottawa) and the contact details of healthcare providers and emergency health services.
- Take note of patients’ preferred phone numbers and emergency contacts in case providers are unable to reach patients directly. Be mindful that the emergency contact that the patient gives during their visits for MA may be different from the emergency contact on file. Be sure not to contact any other individuals without the patient's expressed consent.
Follow-up
The follow-up appointment should be scheduled 3 to 7 days after taking misoprostol (MISO), and more than one follow-up appointment may be needed. The SOGC’s protocol on the provision of medication abortion by telemedicine advises 7 days[7], but some prescribers schedule the follow-up appointment as early as 3 days after MISO administration to avoid loss-of-contact and assess serum bhCG level. The actual practices depend on prescribers’ judgment and experiences.
During the virtual follow-up, prescribers should[7]:
- Review abortion experience and progress with patients, including dates of taking medication, side effects, bleeding pattern, pain, occurrence of expulsion, and any current pregnancy symptoms.
- Advise an urgent assessment or emergency visit if signs of ectopic pregnancy, pelvic infection, heavy bleeding, or excessive pain exist.
- If history suggests failed abortion or ongoing pregnancy: obtain ultrasound and consider an additional dose of MISO or procedural abortion.
- If history suggests successful abortion, no warning signs, and no current symptoms of pregnancy, normal bleeding and pain: arrange the blood test to confirm serum bhCG level if the appointment is in-person or instruct the patient to perform qualitative urine pregnancy test.
Serum bhCG[4]: If the serum bhCG level drops by >50% at Day 3 after MISO or 80% at Day 7-14 after MIFE / MISO administration, the successful completion of abortion is confirmed and no further appointment is needed. Ultrasound should be ordered if 14 days have passed and a drop by 80% has not been reached.
Urine bhCG[7]: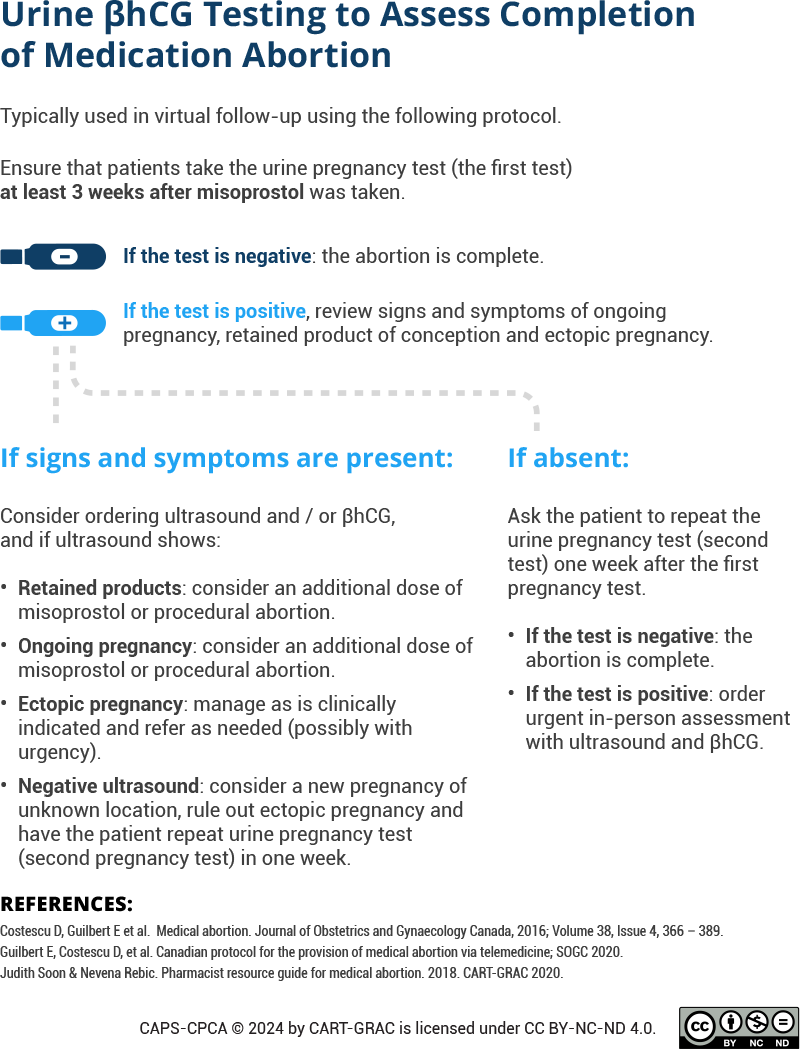
- Offer to discuss contraception options and provide emotional support if needed. Resources for emotional support include:
- Exhale, a talk-line that provides emotional support, resources and information after abortion.
- All-Options, a talk-line to discuss past or current experience with abortion, adoption and parenting for people in Canada and the United States (1-888-493-0092).